SFB 1365 Renoprotection
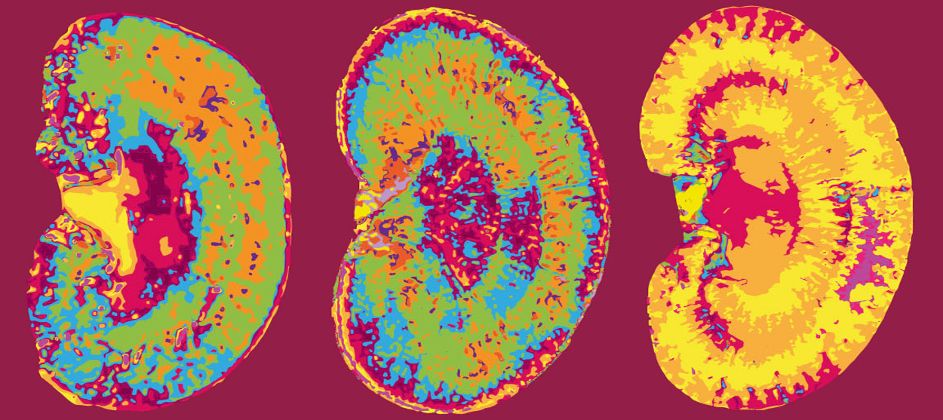
Chronic kidney diseases and acute kidney damage are widespread and reduce the life expectancy of those affected. The CRC “Renoprotection” therefore aims to decode specific signalling pathways for kidney damage and develop new approaches to treatment in the long term (Charité Berlin – FU Berlin and HU Berlin, Spokesperson: Prof. Dr. Pontus Börje Persson).
With the project "Renoprotective role of Lipocalin-2 in allograft rejection following kidney transplantation" Priv.-Doz. Dr. Felix Aigner and Dr. Muhammad Imtiaz Ashraf, PhD will be part of this SFB/CRC!
To provide allograft renoprotection, novel strategies are needed, including (i) prevention of renal allograft IRI and (ii) targeted immunosuppression and thus; reduction and avoidance of steroid and CNI usage in the long-run. Using a mouse model of kidney transplantation, we recently demonstrated a renoprotective role of exogenously administered recombinant Lcn2:Siderophore:Fe complex (rLcn2). The rLcn2 mediated mechanism of allograft renoprotection is still unknown; however, the mechanistic insight is essential for comprehensive translation of the rLcn2 therapy into clinical practice. In the funded project, we aim at (i) understanding the route and mechanisms of immunoregulation and/or cytoprotection, mediated by exogenously administered rLcn2 during the allograft damage; and (ii) characterizing the source and nature of endogenous Lcn2 i.e. whether it is complexed with mammalian iron binding catechols and may contribute to allograft survival in the long-run. Our ultimate goal is to pave the way for transplant renoprotection via recombinant Lcn2.
More information…