We have received the sad news that
Professor Duška Dragun, Director of the Biomedical Innovation Academy (BIA) of the Berlin Institute of Health (BIH) and Head of the Charité BIH Clinician Scientist Program, succumbed to her long, severe, bravely endured illness on December 28, 2020 at the age of 51.
Her tireless efforts were devoted to her life's work: the Charité BIH Clinician Scientist Program. Ten years ago, she launched the first Clinician Scientist Program in Berlin and over the decade established and continuously expanded it as "best practice" for the German-speaking region. She has played a key role in developing and shaping the various programs for scientifically active physicians: from the
Clinician Scientist Program, which enables aspiring specialists to spend up to 50 percent of their working time on research, to the
Junior Clinician Scientist Program with 20 percent working time on research, which begins in the first year of specialist training, to the
Advanced Clinician Scientist Program for specialists with postdoctoral qualifications. Two years ago, she successfully applied to the German Research Foundation (DFG) for the first and only
Digital Clinician Scientist Program in Germany. This enables young physicians and scientists to conduct research and work in the field of digitalization in medicine and healthcare. Thus, within a few years, Duška Dragun made a significant contribution to building a new generation of young professionals for medicine – the impact of her programs will last for a long time, via promising individual careers as well as via the programmatic strengthening of a patient-oriented science.
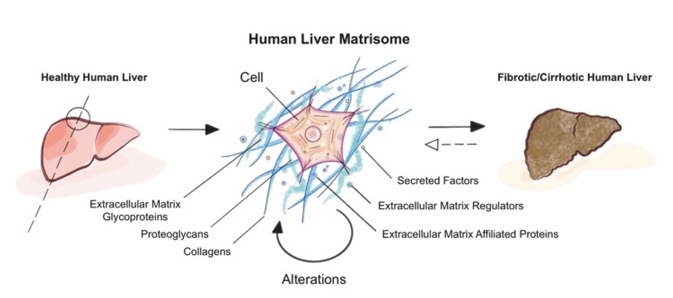
As a physician herself, Professor Duška Dragun has always been committed to research: As acting senior physician and deputy to the acting director of the Department of Nephrology and Intensive Care Medicine at the Charité Campus Virchow-Klinikum, as well as head of the nephrology research laboratory, she made highly regarded, internationally distinguished contributions to transplantation research with the goal of improving graft approach and long-term survival, preventing cardiovascular comorbidity, and thus improving the quality of life and life expectancy of transplanted patients. She pursued her great goals with tremendous energy and passion, impressive perseverance and clear determination. She devoted her full attention to her employees, colleagues, and students, being equally attentive, understanding, and demanding.
The death of Duška Dragun is a great and painful loss. We will miss her greatly as director of the Charité BIH Clinician Scientist Program, as a physician, university professor and scientist. To us she was an inspiration, a mentor and an ever driving force.
Above all, however, we will greatly miss Duška as a friend.